In the healthcare facility, cost efficiency and infection control are two significant factors driving any investment decision.
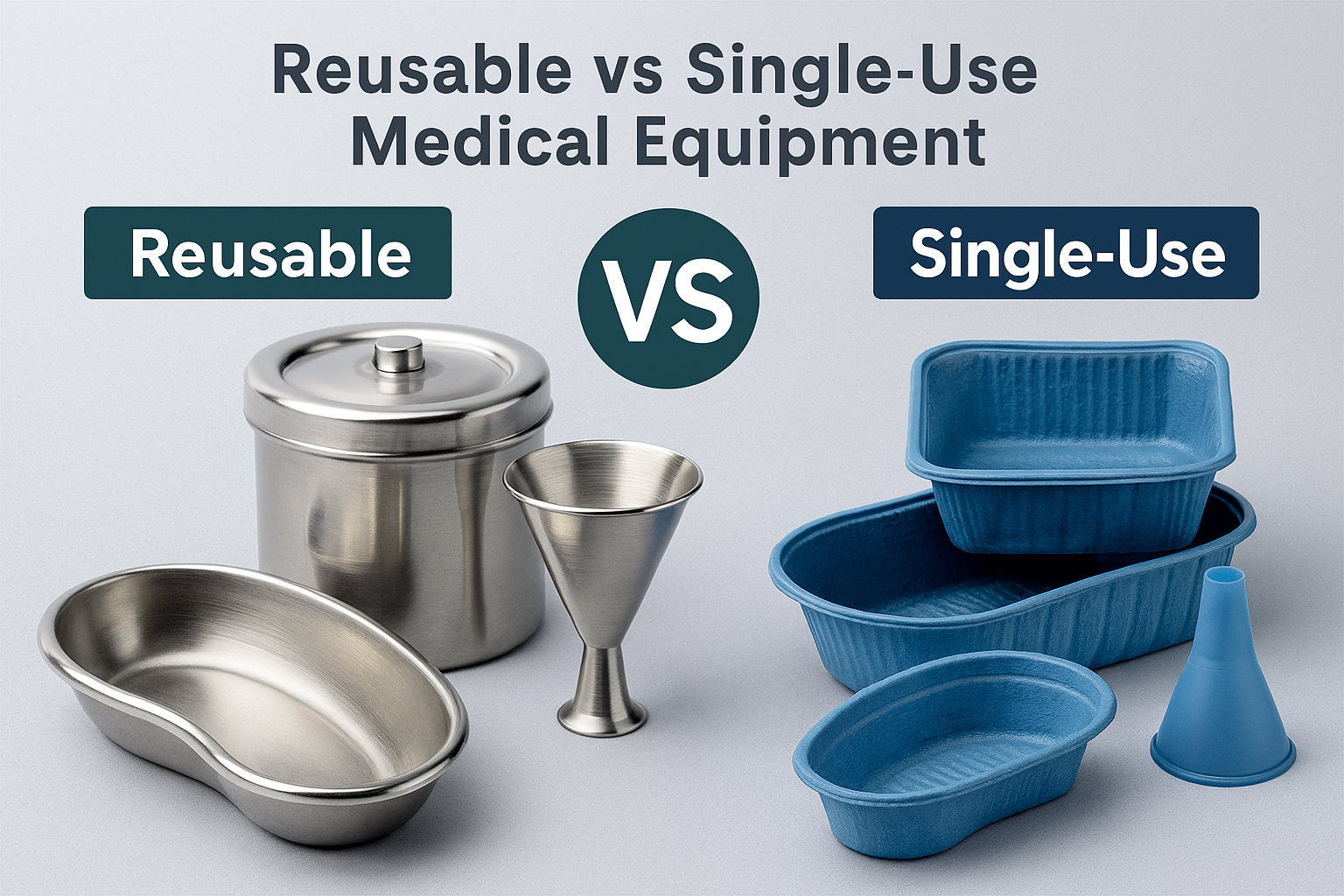
Hospitals, Laboratories and clinics face an important dilemma whether to invest in the reusable medical equipment such as funnels, trays and containers or opt for single-use alternatives.
Both options serve the same purpose; they differ in lifestyle cost, environmental impact and sterilization needs. Understanding these differences helps healthcare facilities and purchasing managers make informed and cost-effective decisions.
What is Single-Use Medical Equipment?
Single-use medical equipment refers to a device that is designed for one-time use on a single patient and then safely discarded. They come pre-sterilized to ensure infection control. There is no need for cleaning or reprocessing them, making them ideal for quick, safe and hygienic procedures. They are made from plastic or lightweight materials.
What is re-usable medical equipment?
Reusable medical equipment is devices designed for multiple uses after proper cleaning and sterilizing them. They are crafted from durable materials like stainless steel or medical-grade polymers.
They maintain their performance over many cycles. The reusable equipment reduces long-term costs and environmental waste in healthcare facilities.
Examples of Re-usable Medical Equipment
- Stainless Steel medical trays
- Medical funnels
- Medical Containers
- Forceps
- Basins
- Tongs
- Scissors
- Basins
Examples of Single-Use Medical Equipment
- Gloves
- Needles
- Cannulas
- Swabs
- Scalpels
- Test Tubes
- Suction Tips
- Pipettes
Cost Comparison – Reusable v/s Single-use Equipment
Re-usable Equipment
- Durable materials like stainless steel or high-grade polymers require higher upfront costs.
- However, these tools are reused for many years after cleaning and sterilization. This reuse reduces the effective cost per use significantly.
- They can last for 5-10 years, depending on the frequency of use and sterilization cycles.
- They have to be cleaned regularly, inspected and sterilized. Trained personnel are required for their effective management.
- There can be costs of repairs or replacement of worn-out items that may occur occasionally; however, the cost per use is low.
Single-use Equipment
- The cost of the initial purchase is low. They are disposed of after single use and are cheaper per unit. They also do not require any initial investment in sterilization, cleaning and trained personnel.
- Continuous procurement increases total cost in a high-volume setting.
- There is no maintenance cost as the single-use tools need not be cleaned and sterilized. They also do not have any handling costs.
- Disposal of the biomedical waste adds financial and environmental costs.
Considering the lifecycle cost of medical equipment, for big hospitals, reusable items are economically smarter in the long term. For small clinics or emergency healthcare facilities, single-use devices are an ideal choice.
Sterilization Challenges in Healthcare Facilities- Reusable Equipment
Sterilization is important to prevent infection. Maintaining sterility for reusable medical items like funnels and trays comes with certain operational challenges-
- Complicated Cleaning Process: Before sterilization, equipment must be cleaned thoroughly to remove biological material. Incomplete cleaning can compromise sterilization, causing cross-contamination risks.
- Complexity: Healthcare facilities use autoclaving, chemical disinfectants or dry heat sterilizers. Each method requires specialized equipment, monitoring and documentation, increasing complications and costs.
- Compatibility: Consistent exposure to high temperature and chemicals can cause warping, corrosion or discoloration in low-grade metals and plastics. The professional manufacturers of medical equipment use only certified medical-grade materials to manufacture reusable equipment.
- Labor and Time Intensive: Manual Cleaning and inspection require trained personnel. This consumes both time and resources. Any errors in handling of the equipment or process timing can cause equipment damage or ineffective sterilization.
Single-Use Devices – Convenience Factor
Single-use disposable medical devices have transformed patient care by simplifying workflows. They are pre-sterilized by the manufacturer; this reduces the burden on sterilization department and reduces the infection risk. The key benefit of the single-use medical equipment includes-
- No Sterilization Delays, thus ideal for emergency
- Consistent sterility eliminates the chances of cross-contamination.
- Simple Logistics, as there is no need for tracking, cleaning or maintenance.
- Improved Safety, making them critical in high-risk departments like ICU or isolation wards.
Sustainability- Environmental Impact
The healthcare industry is a major contributor to the non-biodegradable waste. Reusable equipment supports the global shift towards eco-friendly healthcare, as it reduces landfill waste and carbon footprint. Single–use medical equipment is hygienically safer, but it leads to higher waste volumes and increases incineration emissions.
To create a balance, many modern healthcare facilities are adopting hybrid models, using reusable devices wherever safe and practical, while relying on disposables for specific high-risk or contamination-prone procedures.
Reusable v/s Disposable Medical Devices – Which option is better for your Health Facility
| Facility Type | Recommended Option | Reasons |
| Large Hospitals with CSSD Units | Reusable | Economical in long-term They have good sterilization infrastructure |
| Small Clinics | Single-Use | Reduces Complexity Removes Sterilization needs |
| Mobile and Rural Health | Single-Use | Portability and Hygienic |
| Specialized Surgical Unit | Both | Balances cost, safety and sustainability. |
It is all about choosing the right fit between reusable v/s single medical equipment aligned with your facility’s needs. The reusable equipment offers long-term savings and environmental benefits, but demands a strong sterilization protocol. The single-use equipment ensures quick hygiene and convenience; however, it increases ongoing costs and waste generation.
The best approach is to have a balanced strategy, using reusable instruments where sterilization can be assured and disposable tools where infection risk is the highest. By making informed decisions, healthcare facilities can ensure patient safety, operational efficiency and environmental responsibility – significant pillars of modern healthcare.
FAQs
- Which among the two reusable v/s single-use equipment control infection in hospitals?
United Poly’s single use equipment better controls infection in hospitals as it is used once and disposed of. This eliminates the risk of cross-contamination. - Which is more cost-effective in the long run- Reusable or disposable?
Reusable medical equipment is more economical in the long run despite higher investment. - What are the main challenges of reusable equipment?
They require proper cleaning, sterilization, trained staff and maintenance to ensure safety. United Poly offers the customized and premium-quality reusable medical equipment. - How long does reusable equipment last?
They last for 5-10 years, depending on material quality and sterilization cycles. - Which is better for small clinics or emergency setups?
Single-use equipment is ideal for convenience, hygiene and quick deployment. United Poly manufactures and exports the premium quality disposable medical instruments.